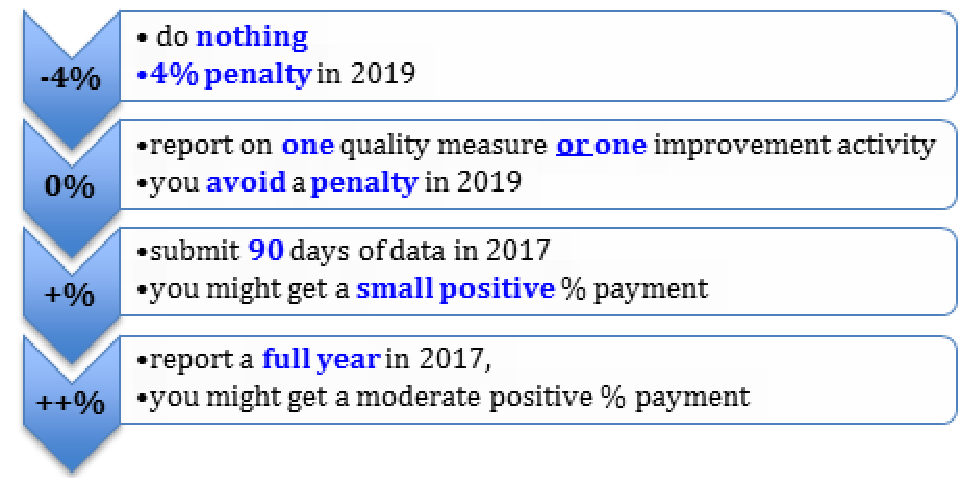
Starting in January 2017, your practice needs to do something to avoid up to a 4 percent penalty in 2019. At KMA, we are trying to get the information to you to download, put in a binder, label MACRA, and have ready for quick reference to avoid penalty cuts. Follow these five easy steps.
Step One
Copy/download the article from our October Newsletter to have the terminology and explanations handy.
Step Two
If this is your very first year participating in Medicare, you are not required to participate in MIPS.
Step Three
The New Rules—released Oct. 14, 2016—say if your practice has less than $30,000 in allowed Medicare charges OR sees less than 100 Part B enrolled Medicare patients YOU ARE EXEMPT from the MIPS rule, although the exemption may have to be reported. Stay tuned for how to report the MIPS exemption.
Step Four
If you are part of an APM (Alternative Payment Model), you are exempt from MIPS. There are very few APMs in Kentucky. Learn more about Alternative Payment Models such as Accountable Care organizations and other innovations in Kentucky.
Step Five
The Medicare Quality Payment Program website helps you:
- Decide to participate in MIPS as an individual or group
- Explains the four categories that you will be scored on
- Locate quality measures applicable to your specialty to report for the quality category
- Select up to four Clinical Practice Improvement Activities to report A PCMH designation provides you full credit in this category (Tip: A PCMH designation provides you full credit in the CPIA category)
- Select measures for the Advancing Care Information category – reminder the Electronic Health Record (EHR) that you use must be certified

