On June 11, 2021, the U.S. Department of Health and Human Services released revised reporting requirements for health care providers who received Provider Relief Fund (PRF) payments. These revisions expand the amount of time providers have to report information and extend key deadlines for expending PRF payments for recipients who received payments after June 30, 2020. The revised reporting requirements are applicable to providers who received one or more payments exceeding $10,000, in the aggregate, during a single Payment Received Period from the PRF General Distributions, Targeted Distributions, and/or Skilled Nursing Facility and Nursing Home Infection Control Distributions.
Other key updates include:
- The period of availability of funds is based on the date the payment is received rather than requiring all payments be used by June 30, 2021, regardless of when they were received.
- Recipients are required to report for each payment received period in which they received one or more payments exceeding, in the aggregate, $10,000 rather than $10,000 cumulatively across all PRF payments.
- Recipients will have a 90-day period to complete reporting as opposed to the original 30-day reporting period.
- The PRF Reporting Portal will open for providers to start submitting information on July 1, 2021. Providers are encouraged to register in the PRF Reporting Portal now.
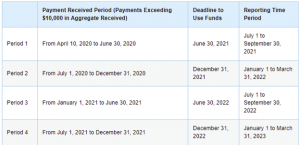
The table below summarizes the payment received periods with the corresponding deadline to use funds and reporting time period:
For additional information on the revised PRF reporting requirements, please see the following resources:


