Merit Based Incentive Payment System (MIPS) Phase One – Proposed Rule
Physicians will have until 5 p.m. June 27 to comment on a proposed rule regarding the new Merit-Based Incentive Payment System, known as MIPS. The Centers for Medicare & Medicaid Services released the Rule on April 27.
Congress eliminated the Sustainable Growth Rate (SGR) last year; that change started the transition to the new Merit-Based Incentive Payment System. When this system takes effect, physicians may receive payment adjustments to their fee-for-service Medicare payments through participation in the MIPS program or in a qualifying alternative payment method on or after Jan. 1, 2019. Physicians may choose MIPS or an alternative payment method but cannot participate in both, although Medicare will permit physicians to switch methods from year to year.
Currently, Medicare measures the value and quality of care provided by physicians and other clinicians through a mixture of programs, including the Physician Quality Reporting System (PQRS), the Value Modifier Program and the Medicare Electronic Health Record Incentive Program. Beginning in 2019, Medicare will consolidate the three existing incentive programs – PQRS, Meaningful Use (MU) and Value Based Payment Modifier (VBPM), and continue to focus on quality, resource use and meaningful use of electronic health records through MIPS.
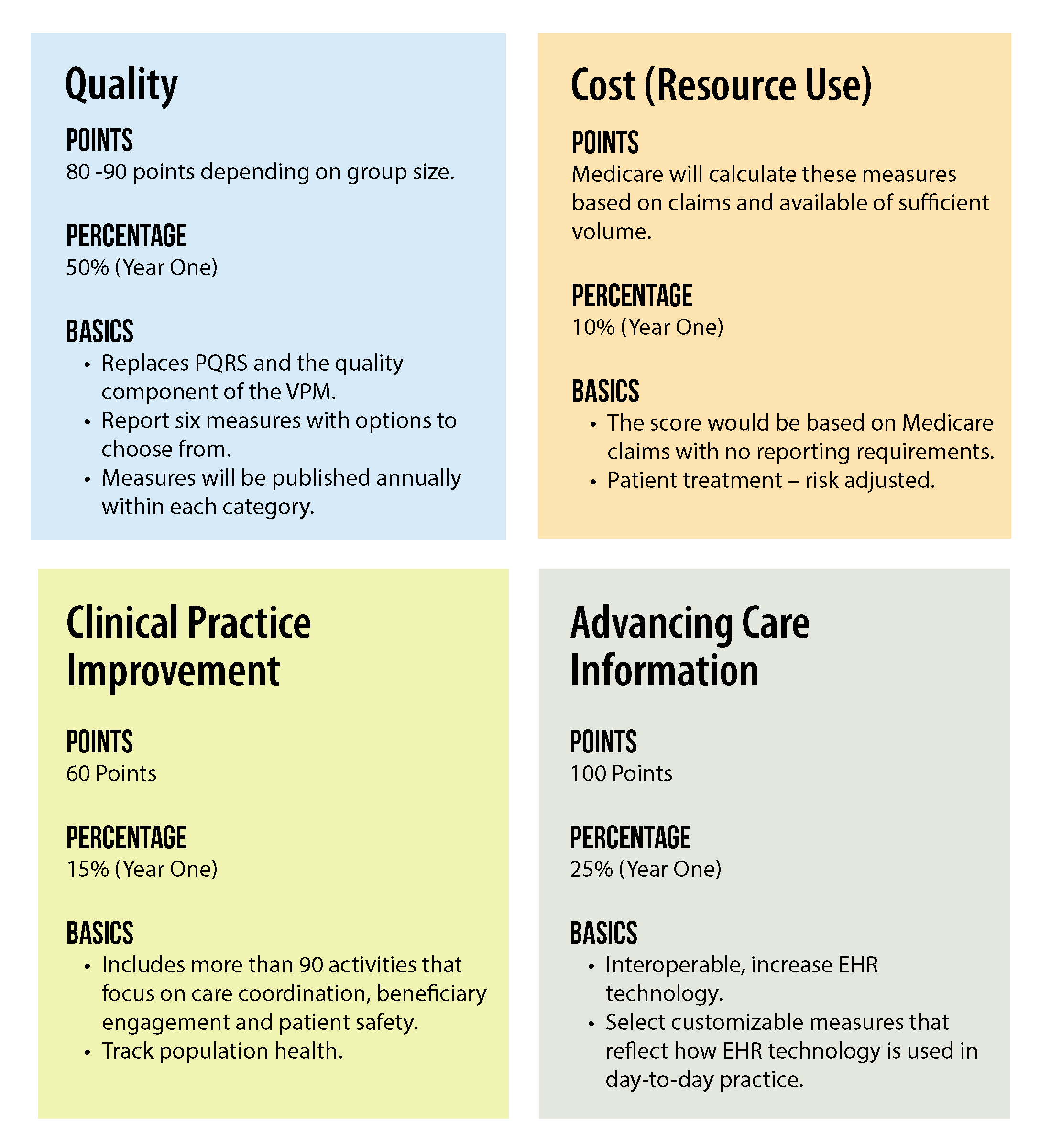
Physicians and other eligible clinicians will receive a composite performance score of 0-100 based on their performance in each of the four categories used in MIPS – quality, cost (resource use), clinical practice improvement and advancing care information. The performance standards for all measures and activities will be calculated for a calendar year Jan. 1 through Dec. 31. Each standard will be calculated by category on a percentage basis.
Many physicians will be impacted by MIPS with a few exceptions still being defined by Medicare. The exceptions may include: physicians newly enrolled in Medicare (first-year physicians); physicians with low volume threshold (have less than or equal to $10,000 in Medicare charges and less than or equal to 100 Medicare patients; or physicians who are significantly involved in participating in an advanced alternative payment model.
MIPS scores are used to compute a positive, negative or neutral adjustment to their Medicare Part B payments. In the first year, depending on the variation of MIPS scores, adjustments are calculated so that negative adjustments can be no more than 4 percent and positive adjustments are generally up to 4 percent. Both positive and negative adjustments would increase over time. Additionally, in the first five payment years of the program the law allows for $500 million in an additional performance bonus for high performers.
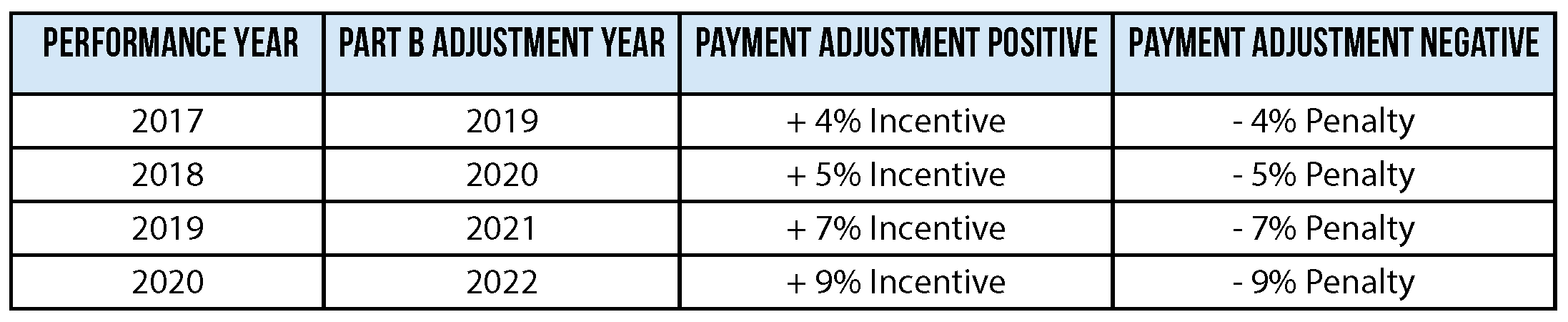
- Physicians with high composite scores will be eligible for a positive payment adjustment that is up to three times the baseline positive payment adjustment for a given year (2020 Performance Year Max Base Incentive: 9% x 3 = 27%).
- Physicians who do not report any MIPS quality metrics will automatically be given the lowest score. See the maximum downward adjustment, unless one of the applicable exceptions (still being defined by Medicare) applies.
- Physicians that elect to participate in an APM could receive an upward payment adjustment of 5 percent for up to 6 years and if the practice is a certified patient centered medical home, could earn more (15%) since the risks are greater. Medicare has not yet defined how much financial risk physicians must take – only that it will be a “generally applicable financial risk.”
Another component of MIPs – the Physician Compare website – will publish physician MIPS scores in each category. For the first time, Medicare consumers will be able to see how their physician compares with other physicians throughout the nation on how they are doing improving patients health, use of electronic records, electronic prescribing and more.
KMA will continue to update members with more details on this important subject. If you need help providing a comment on the Proposed Rule, have questions or want more information on this topic, contact KMA at lady@kyma.org.

