The CARES Act includes relief to health care providers, including physician practices, who are suffering financial loss due to COVID-19 by designating $100 billion funding for the Department of Health and Human Services (HHS) Public Health and Social Services Emergency Fund. The statute requires HHS to interpret eligibility for the funding broadly to include all physicians who are experiencing revenue losses and non-reimbursable expenses as a result of the COVID-19 pandemic.
KMA has produced a one-page handout, available here, for physicians regarding details about the allocation of these funds. The information is available to members as an informational resource. KMA expresses no opinion as to the feasibility, applicability, or impact to your particular practice.
CGS Webinar on Accelerated/Advance Payment Program
CGS Administrators, LLC (CGS), which provides a variety of services for Medicare beneficiaries, healthcare providers, and medical equipment suppliers in a number of states, including Kentucky, will host a webinar on the Accelerated/Advance Medicare Payment Program tomorrow, April 14 at 1:00 p.m. (ET). CMS has expanded the current Accelerated and Advance Payment Program during the COVID-19 public health emergency to extend financial hardship relief to impacted Medicare Part A Providers, and Part B Providers/Suppliers. CGS staff will provide an overview of this expansion, provide step by step instructions and address questions. Registration is available online at https://register.gotowebinar.com/register/7098879583080721932.
Last week, KMA released an informational resource, available here, regarding what physicians need to know about the Accelerated and Advance Payment Program process.
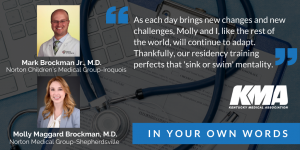
In Your Own Words: Mark Brockman, Jr., M.D. and Molly Maggard Brockman, M.D.
KMA is sharing the first-person accounts of physicians from across the state as they prepare for and battle the COVID-19 pandemic. These stories will also be published at kyma.org/covid19. If you are interested in submitting an account, please email Emily Schott, schott@kyma.org.
 As a physician couple, my wife Molly and I have been through some uncertain and stressful times together. We met nine years ago in medical school and survived the stressors on our relationship that only fellow physicians would understand: surviving Step One (and two and three), couple’s matching, the crazy schedules, the stress of residencies, and passing boards. But we got through it all, together, and our marriage emerged stronger than ever.
As a physician couple, my wife Molly and I have been through some uncertain and stressful times together. We met nine years ago in medical school and survived the stressors on our relationship that only fellow physicians would understand: surviving Step One (and two and three), couple’s matching, the crazy schedules, the stress of residencies, and passing boards. But we got through it all, together, and our marriage emerged stronger than ever.
We were looking forward to settling into our lives as community physicians in the Louisville area and finally doing things that normal couples get to do. But now we’re faced with the most uncertain and trying time of our career: our first (and hopefully last) pandemic as a pediatrician and med/peds physician.
These past few months have left me wondering where we will be when the smoke clears. We all see the news of front-line workers helping our communities, sometimes at the sacrifice of their own personal protection. Currently, we’re on the hospitalist reserve list for potentially being pulled to those front lines, but for now, in the outpatient world, our view is very different.
Honestly, I still had influenza and RSV on my mind when we started talking about COVID-19 coming to Kentucky. As the days went on, I began to receive texts and calls from friends and family and countless patient questions about my opinion on the matter. It’s frustrating when you studied so hard in your career to obtain knowledge about various diseases and feel so clueless about such a societal dismantling virus. Our community and patients look to us to offer knowledge and guidance. I find myself saying, “I don’t know” when asked how long this will last or how the virus impacts child safety. Learning how to direct a discussion about COVID-19 to certain age groups has been challenging. We’ve both added time to our visits for extra conversation.
Although the CDC and NIH provide good information, the talks with my wife at the dinner table are perhaps the most helpful. We exchange articles we’ve read about the epidemiology, the ever-evolving knowledge of the pathophysiology, and possible treatments. Our texts used to consist of funny memes but now are an exchange of medical articles that offer more insight.
Right now, I can’t image not having a partner that knows exactly how exhausting it is for a primary care doctor right now; adapting to the ever-changing policies and CDC updates, fielding calls from family and friends, trying to comfort anxious patients while simultaneously wondering if things really are going to be okay. I’ll never forget the 7-year-old girl in my office, clinching a handful of masks to take back home to “protect her family.” Now, our protective gear is stashed away, only to be used judiciously.
We’ve both been impressed with how quickly our practices have adapted schedules and implemented new policies. As with most primary care offices, we’ve seen a decline in patient numbers. This brings up so many questions: Are people staying home with things they normally need to come in for? Are kids not spreading germs with the new social restrictions in place? Are the decreased office visits hurting patients in the long run? What’s happening to routine vaccine schedules, antibiotic stewardship, and patients with uncontrolled chronic illness during this time? Will we eventually see a primary care surge after COVID-19 dies down to catch up on what has been put off during this quarantine time? Will we see a surge of COVID patients?
One thing is for sure, offices have changed rapidly. To save PPE, physicians have been triaging and obtaining vitals and labs on all sick patients. Molly, also being an internist, has had many patients hospitalized and a death due to COVID-19. We have been chart-checking more from home as the amount of inbox messages have increased. This brings up a new challenge of triaging potentially sick patients through messages and phone calls because they do not want to come into the office. We’ve also implemented telemedicine at the office and, possibly soon, telemedicine from home. Hopefully, the patients won’t mind my hound dogs howling at the barn cats in the background.
As each day brings new changes and new challenges, Molly and I, like the rest of the world, will continue to adapt. Thankfully, our residency training perfects that “sink or swim” mentality, which is coming in handy now. We’ll continue to provide the best care we can for our patients and come home at the end of the day to care of each other, just as we have since medical school. I have no doubt this experience will have an ever-lasting impact on our careers, and we will be better physicians because of it.


