Two out of three Medicare beneficiaries today have two or more chronic conditions, and one out of three have four or more chronic conditions. Those combinations of conditions often make it difficult to coordinate care and improve the health of the patient.
Recognizing that care management is a critical component of primary care, the Centers for Medicare and Medicaid Services (CMS) introduced a non-visit based payment for chronic care management as part of its Merit-Based Incentive Payment System, or MIPS. The system is the result of consolidation of three existing incentive programs—Physician Quality Reporting System, Meaningful Use and Value Based Payment Modifier. The previous all or nothing approach will be replaced with a single composite score (01-100) that will factor performance in four weighted categories—Cost, Quality, Advancing Care Information, and Clinical Practice Improvement Activities.
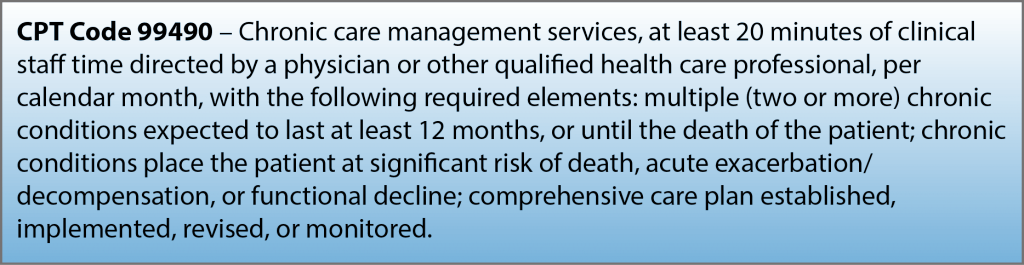
Under the new non-visit based payment, Physicians receive a monthly fee of around $41 per beneficiary when caring for patients who have two or more chronic conditions that are expected to last at least 12 months and/or place the patient at significant risk of death, decompensation or functional decline.
The modest fee can improve reimbursement for physicians; for example, 200 qualifying patients could add about $100,000 annually in income.
To bill for this service, physicians are required to use a certified electronic health record (EHR), offer round-the-clock access to staff who have access to the EHR, maintain a designated practitioner for each patient, and coordinate care through transitions to and from the hospital and specialists.
The chronic care management program potentially could improve care coordination, even keeping the patient out of the hospital, and would help meet the clinical practice improvement activities category requirement of MIPS.
Contact KMA with questions about the clinical practice category or the chronic care management program at lady@kyma.org.
Clinical Practice Improvement Category
The clinical practice improvement category accounts for 15 percent of the MIPS score in the first year. For this category, MIPS would reward clinical practice improvement activities focused on care coordination, beneficiary engagement and patient safety.
Physicians would select from a list of more than 90 activities updated annually from broad categories that include:
• Expanded Practice Access
• Population Management
• Care Coordination
• Beneficiary Engagement
• Achieving Health Equity
• Emergency Preparedness and Response
• APM with Medical Home Model
• Integrated Behavioral and Mental Health
Click here for a listing of all 90 activities.
The maximum total in this category is 60 points, and the score is determined by weighting the reported activities. Highly weighted activities would be worth 20 points, while other activities would be worth 10 points.
Examples of highly weighted activities are the collection and follow-up on patient experience or seeing Medicaid patients in a timely manner. Use of telehealth and chronic care management may indicate care coordination, while smoking cessation and medical nutrition therapy may count toward engaging the patient in decision-making.
NOTE: This is the second in a series of KMA web-based MIPS resources. Other topics in the series:
• “Important Changes—Physician Reimbursement”
Click here for printable Resource guide for this article.


