Posted October 5, 2018
Submitted by the American Medical Association
The prevalence of type 2 diabetes has been rising over the past 20 years. Based upon statistics on current health trends from the Centers for Disease Control and Prevention (CDC), it is estimated that 30 million adult Americans have diabetes1, or approximately 10% of the adult population.
Even more adults are at risk for developing type 2 diabetes; the CDC estimates that currently 84 million adult Americans have prediabetes1, a condition in which glucose levels are higher than normal but not high enough to diagnose type 2 diabetes. Prediabetes can be a reversible condition and treating it can delay or prevent progression to type 2 diabetes. However, the majority of adults who have prediabetes are unaware of their condition.2
The National Diabetes Prevention Program lifestyle change program (National DPP lifestyle change program) is a structured, year-long program that has been proven to help patients delay or prevent type 2 diabetes. Over the past few years, the CDC, the American Medical Association (AMA), and healthcare organizations across the nation have worked together to bring National DPP lifestyle change programs to patients.
The following three steps can help you identify patients with prediabetes and refer them to a National Diabetes Prevention Program lifestyle change program.
Step 1: Identify patients with prediabetes
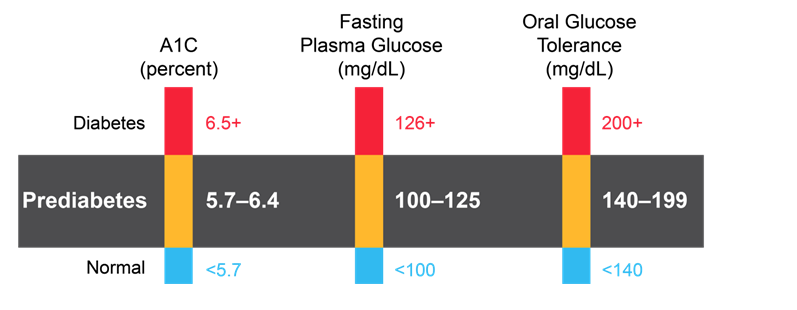
Prediabetes can be diagnosed through one of three laboratory tests-the hemoglobin A1C, the fasting plasma glucose or the oral glucose tolerance test. The diagnostic ranges for normal glucose, prediabetes and type 2 diabetes are in the figure below3:
Risk factors for prediabetes mirror those of type 2 diabetes and include a BMI that is consistent with overweight or obesity, among others. The United States Preventive Services Task Force has a screening recommendation4 for abnormal glucose in adults, or you can use an alternative screening protocol. For patients who have had a recent laboratory test, you can use your electronic health record or laboratory reports to identify those who meet the diagnostic criteria for prediabetes. Once patients with prediabetes have been identified, patients should be informed of their diagnosis, either during their next office visit or through an established notification process. This diagnosis should be documented in their chart, you can use the ICD10 code R73.03 to document prediabetes.
Step 2: Provide patients with evidence-based treatment
The National Diabetes Prevention program lifestyle change program is an effective and evidence-based treatment for patients with prediabetes that has been proven to delay or prevent type 2 diabetes5. The program is an intensive lifestyle change program that can be delivered in-person, through distance learning or through virtual modalities. Individuals participate in group sessions led by a trained lifestyle coach that take place on an approximate weekly basis for the first few months of the program and then transition into a maintenance phase, which consists of sessions approximately once a month. The curriculum is comprehensive and gives participants the knowledge and skills to make sustainable healthy lifestyle changes. The curriculum includes topics on healthy diet and physical activity, as well as stress management and behavioral strategies to make lasting changes. The CDC provides oversight and quality assurance of the National DPP lifestyle change program and maintains standards for program sites to receive approval and recognition. You can find program locations near you on the CDC’s National Diabetes Prevention Program website. https://nccd.cdc.gov/DDT_DPRP/Registry.aspx
Step 3: Monitor and follow-up
If you refer patients to a National DPP lifestyle change program, it is recommended that you monitor their progress and follow-up on their outcomes to help support them. A process should be established with the provider of the National DPP lifestyle change program to share regular updates about participation and achievement of goals for patients in the program. It is recommended that communication occur at designated points during the program. This will also allow you to arrange any appropriate follow-up visits or repeat laboratory testing for patients.
By using these three steps, you can help your patients reduce their risk of developing type 2 diabetes and make them aware of the National DPP lifestyle change program. As a result, you empower your patients to improve their health and provide them with the skills and strategies to make long-term healthy lifestyle changes.
For more information, consult the Prevent Diabetes STAT toolkit, which includes patient identification/management protocols, referral templates and patient awareness and education materials.
Your participation in a brief survey regarding this article on prevention strategies for type 2 diabetes would be greatly appreciated. To complete the survey, use the link below.
https://survey.az1.qualtrics.com/jfe/form/SV_cTSthJYUMozHZ7T
References
- The Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2017: Estimates of Diabetes and Its Burden in the United States.
https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf.
Accessed October 1, 2018
- Centers for Disease Control and Prevention, Awareness of prediabetes-United States, 2005-2010, MMWR, Morb Mortal Wkly Rep 2013;62(11) 209-12.
- American Diabetes Association. Section 14. Diabetes Advocacy. Standards of Medical Care in Diabetes – 2016, Diabetes Care 2016:39(Suppl 1)S105-S106).
- Siu AL Peters JJ, Bibbins-Domingo K, Grossman D, et al.. Screening for abnormal blood glucose and type 2 diabetes mellitus: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;163:861-8.
- Knowler WC, Barrett-Connor E, Fowler SE, et al. Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002; 346(6):393-403.